Have You Met Mark?
Mark Fetterman lives near our Clinic and supports our work because he knows the positive impact we have in the lives of our patients. Read his inspiring story about how he actively chose to not let his cleft define his future. I was born in 1971 in Wilmington, Delaware with
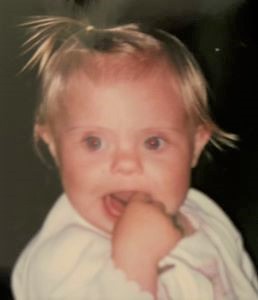
Have You Met Leah?
Leah was born with Down Syndrome. And it was a surprise to her parents. All they want is for her to be happy, but she really struggled to eat as a baby. Leah could nurse, but bottles didn’t work and a pacifier was never comforting. Imagine not being able to
Tuesdays with Nola
Team Tuesdays can be stressful with so many patients and their families visiting the Clinic on the same day. Sometimes our longtime volunteer, Joni, will bring Nola to visit with patients. Nola is a King Charles Spaniel with the perfect disposition to bring calming joy on a busy day. Joni
Fresh Paint!
Our renovation is nearing a close, and the fresh paint on our building exterior is the latest evidence. Here’s a rather astounding “during” and “after” so you can enjoy the transformation.
Atrium and Elevator are Complete!
Our new atrium entrance and elevator are in place! The new entry is open for use now, and the elevator will be ready after inspections.
New KidZone is nearly complete!
The new KidZone is nearly complete! Our playhouse has taken shape, and we have fluffy white clouds suspended from the ceiling. This creative accent gives the room dimension, plus helps reduce noise.
Removing an Unexpected Oil Tank!
Here are photos of our new elevator and main entrance, PLUS the removal of an old (unknown!) fuel oil tank. Staff reports that the building shook when it was yanked out!
New Mural in the KidZone Play Area
Watch as our beautiful landscape comes to life!
New Equipment Moves In!
Plus clinical workroom, elevator, hallway, conference room, offices, and research center!
Creating Confidence Through Clear Communication
Fall 2020 Newsletter Released LCPC is excited to announce that our speech pathology department is growing! Brittany Bilitzo will be joining Pilar Tobin on our team of speech and language pathologists in our expanding department. Brittany, an MS CCC-SLP, comes to us from Nationwide Children’s Hospital in Ohio where she completed a